EHR adoption has become a requirement in the United States. Not implementing an EHR will bring financial penalties for non-compliance. The medical center executives are looking to mitigate risks and ensure the success of the implementation. This guide contains steps to help them do so. It is based on our 4+ years of experience with developing custom EHRs and EMR systems, official recommendations from the USA government and other reliable sources.
Contact us to learn how our EHR experts could help you with EHR transitioning and selection, EHR implementation, training or support!
The cost of implementing an EHR system
EHR adoption and implementation costs include purchasing and installing hardware and software, converting paper charts to electronic ones, and training end-users. The maintenance of an EHR can also be expensive. In fact, physicians frequently cite upfront costs and ongoing maintenance costs as the largest barriers to the adoption and implementation of an EHR.
The financial incentives built into the HITECH Act are designed to defray some of the costs associated with EHR adoption, especially for smaller organizations. Physicians with more than 30% of their patients paying with Medicaid are eligible for up to US$63,750 in incentives over a 6-year period. On the other hand, physicians accepting more Medicare patients are eligible for up to US$44,000 over a 5-year period as long as they can meet the “meaningful use” criteria starting the first year. Hospitals are also eligible for incentives under the HITECH Act. The base amount to each hospital that complies with the meaningful use criteria will be more than US$2 million.
Request a custom price quote for your EHR System. Use the form with EHR Features list here to describe the project and we will get in touch with you within 1 business day.
EHR Implementation Case Study: HealthTexas Provider Network
The total cost of implementation of an EHR for a five-physician practice through the first year was $232,885 (including maintenance costs). The trusted source
EHR Implementation Cost Breakdown
|
Expenditures |
First-year costs |
|
Hardware costs (fixed) |
$25,000 |
|
Hardware costs (variable) |
$35,290 |
|
Software license, hosting, etc. (variable) |
$85,500 |
|
Network implementation team (fixed) |
$28,025 |
|
Practice implementation team (fixed) |
$7,413 |
|
Practice end-user (variable) |
$51,657 |
|
Total per practice |
$232,885 |
|
Total per physician |
$46,577 |
EHR Implementation Case Study: Belleville Family Medical Clinic
The total cost of implementation of an EHR for practice with six resident physicians through the first year was $220,800 – $260,800 (including technical support). The trusted source
EHR Implementation Cost Breakdown
|
Expenditures |
First-year costs |
|
Vendor costs: software, interface, training |
$51, 500 |
|
Hardware costs: database server, desktop computers, printers |
$67,000 |
|
Other costs: wiring, remodeling, surge protectors, etc. |
$12,000 |
|
Project manager: half time for nine months |
$24,000 |
|
Project team: a portion of regular compensation accounted for by estimated time devoted to the project |
$60,000 – $100,000 |
|
Training time: staff |
$6,300 |
|
Total per practice |
$220,800 – $260,800 |
|
Total per physician |
$36,800 – $43,467 |
EHR Implementation Case Study: 14 solo/small-group primary care practices in 12 states
The financial costs (min-max) per FTE physician per year was $20,419-75,567. Variations in financial costs reflect exceptional heterogeneity among small practices in pre-EHR hardware and in technical and negotiating skills. The trusted source
EHR Implementation Cost Breakdown
|
Expenditures |
Financial costs (min-max) per full-time equivalent (FTE) physician per year |
|
Software, training, and installation costs |
$8,475 - $32,607 |
|
Hardware costs |
$5,261 - $23,600 |
|
Revenue losses from reduced visits during training and implementation |
$0 - $20,000 |
|
Software maintenance and support |
$1,200 - $3,800 |
|
IS staff and external IT contractors |
$0 - $5,556 |
|
Initial data abstraction costs and extra telecommunication costs. |
$0 - $12,394 |
|
Total per physician |
$20,419-75,567 |
- Software included license or maintenance costs for EHR or related software (for interfaces, databases). Installation included vendor and contractor costs for installing software.
- Hardware included computer equipment (desktop computers, laptops, servers, storage), related ancillary equipment (printers, scanners, monitors), and networking (routers, wiring).
- Revenue losses at implementation were attributable to provider productivity decreases resulting from reduced visit schedules.
- IS staff and external IT contractor costs included increases resulting from the EHR.
EHR Implementation Plan
To ensure efficiency, there is a series of steps the provider’s staff must follow to ensure proper implementation and handling of the EHR system.
1. Assemble the implementation team
These people will make sure the new EHR is adopted on time and budget. The team should include medical professionals, administrators, compliance specialists and technical specialists (if applicable to your practice). The American Medical Association (AMA) recommends to appoint people to three key positions:
Project Manager
The PM’s primary job is to serve as a liaison between the practice and the EHR vendor. Their duties also include monitoring the project timelines and running the day-to-day activities of the team. A PM could be either a member of your own team, a vendor’s employee, or a third-party specialist.
Lead Physician
This position should be occupied by a medical professional, preferably from your own hospital. A Lead Physician should make sure that the needs of doctors and nurses - the end users of the new EHR - will be addressed during the implementation process.
As building a custom EHR implies working with a focus group from clinical staff members to gather requirements and test the system, a person from that group would make a great Lead Physician. They already have experience in communicating their needs and providing feedback.
Lead Super User
The Lead Super User should be a tech-savvy person who knows the clinical workflow of your practice. Whenever a medical professional has a problem with the new EHR this is the person they contact. The Lead Super User along with their team (in larger practices) will have received training with your custom system and will transfer this knowledge to their coworkers. There should be at least one super user for each of your offices.
In small organizations, this position could be combined with PM. This is also true for implementing custom-built EHRs, as the creation of forms and workflows would be done at the development stage.
The Office of National Coordinator for Health IT (ONC) suggests a similar approach, but defines a more extensive leadership team, including Nurse Champion, Lab Staff Lead, Billing Lead and others. Whether you do need to fill those positions depends on your organization’s circumstances and goals.
2. Adapt workflows
AMA strongly recommends reviewing your clinical workflows before implementing a new EHR. Otherwise, the problems caused by their inefficiency will only get worse.
As this is a medical issue and not a software-related one, your doctors and nurses would be far better qualified to give you advice on how to proceed with changing the workflows. The EHR can and should be adapted to accommodate them.
3. Prepare the Hardware
This stage includes preparing all the physical tools that will work with the EHR, from the servers (if you’ve chosen an on-premise system) to the tablets, desktop computers, and patient-facing registration screens. It is typically done either by the practice’s in-house IT team or by a third-party company, independent from the EHR provider. If there is a need for it, the same company can also be hired to provide continuous hardware support.
Off-the-shelf systems have a set of technical requirements that the vendor will give you, while in custom EHRs this matter would be discussed between you and the development company in advance.
4. Customize EHR software
Even if the EHR you’re implementing is tailored to your medical specialty (e.g. orthopedics or mental health), it needs extra tuning to adapt to your practice’s workflow. This part also includes ensuring whether your software provides adequate protection of the patients’ data, so feel free to check out our HIPAA-compliance checklist.
In turnkey systems customization starts before the actual development process and is included in the quote. The contractor works with a focus group of stakeholders (typically, clinical and business staff) to determine the challenges and ways to solve them. Then, over the course of the development process, this group tests the system’s functionality and provides feedback so that it can be improved. As a result, the EHR is form-fitted to your practice’s needs and a number of core personnel are already familiar with it, decreasing the time needed for training.
In off-the-shelf EHRs this is done in the beginning of the implementation stage. The vendor’s team will adapt their product to your requirements and workflows. The costs will depend on the rates of the company that supplies your EHR.
5. Migrate Information
This stage includes the transfer of both clinical (diagnoses, treatment plans, allergies, etc.) and non-clinical (e.g. insurance) data from your old system to the new one. Transition is risky - corrupted or incomplete records might deny your employees access to the new EHR’s functions or even present a health risk to your patients (especially in case of allergy or drug interaction information).
ONC makes a compelling case for tasking your outgoing vendor with data transfer and even suggests including it as a provision in your contract right from the start. Besides saving you money and giving you confidence, this way you won’t become hostage to the inefficient system, should you decide to switch to a different provider later.
The information should be presented in an accessible way, for example FHIR format, so that the new provider can easily migrate it to their system. Alternatively, the outgoing vendor can give you the documentation and/or software that will allow your in-house specialists or the incoming vendor to handle the transfer themselves.
As the change takes time, make sure to keep access to your old EHR until your new system is up and running, so you will be able to continuously provide care to your patients. You should also check whether you are legally required to maintain access to the old records, as this varies depending on the state you’re based in. For example, Indiana requires keeping the records for 7 years, while in neighboring Ohio the healthcare provider “must retain medical records for 6 years since the date of discharge”.
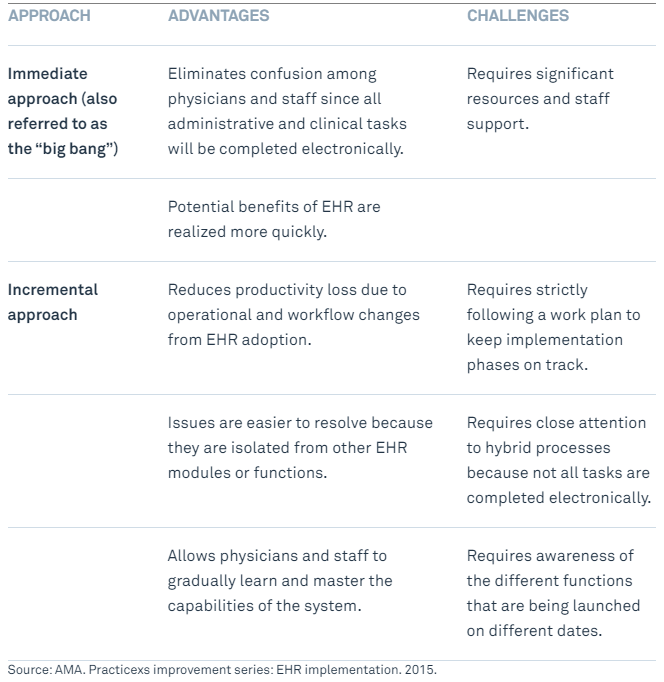
6. Choose the implementation strategy
There are two major approaches to adopting a new EHR, whether you are switching from the old system, or implementing a new one from scratch: “The Big Bang” (immediate approach) and incremental.
Both have their inherent pros and cons.
7. Plan for downtime
You can have the most secure and reliable EHR possible, but it is all for naught if your internet cable is cut by a stray excavator or the power is out due to a hurricane or ice storm. Your provider might discover a security vulnerability that requires an immediate fix. Or shutting the system down might be necessary in the case of a cyberattack to control the damage from it.
That’s why your practice needs to prepare procedures for both planned and unplanned EHR downtime. It can be a part of a Medicare-required continuity of operations plan.
The emergency procedures should cover communication with the staff and the patients, patient processing, documentation, billing, prescriptions, and procedures for entering the information back into the EHR once it’s up again. Each location in your practice needs a copy of the plan (or several).
While the organizational issues would be better addressed by your practice’s leadership, your EHR vendor can help set up the backup procedures and assist in restoring the information.
As with other emergency procedures, you should periodically conduct drills so your staff is prepared for the moment the real disaster strikes.
8. Conduct EHR training
ONC recommends three ways you can teach your employees to work with a new EHR:
- Super users. This is a trickle-down approach, which implies training a core group of employees that will, in turn, train their coworkers.
- Role-based. Everyone gets the training depending on their position within the practice: doctors learn only the part related to patient processing; billing staff - financial reporting, payments, insurance etc.
- Process-based. “Suppose we have a patient complaining about his broken leg. This is how we would handle it with the new EHR…”
Off-the-shelf systems providers have knowledge bases that are accessible to their customers and dedicated implementation specialists to conduct onsite and offsite training.
A custom EHR development company, like ours, can set up online courses to help with onboarding of your current and future staff.
How We can help with implementing a custom EHR
- Data migration. We can work together with your outgoing vendor to speed up the transfer of records from your old system to the new one.
- Backup procedure preparation. We can advise you on how to make your system ready for emergencies and quickly restore lost data in case of malicious acts.
- Super user training. We thoroughly document the software we build and can use it to teach the core group of your employees who will then impart their knowledge on their colleagues.
- Long-term education and onboarding. We can set up a complete training course that will help your current staff refresh their knowledge of your custom EHR and your new employees to quickly become proficient with the system.
Additional resources
- The ONC Health IT Playbook contains extensive information on EHR implementation, including sample articles for contracts with a vendor, data transfer advice and workflow optimization.
- AMA has a training module dedicated to switching from paper records to EHR.
- The HIPAA compliance checklist will help you secure both the EHR and your practice in general.
- The GDPR-compliance checklist is applicable to organizations processing the information of EU citizens, but also contains useful data security practices.
Rate this article
Recommended posts
Portfolio
Our Clients' Feedback




















.jpg)
.jpg)













Belitsoft has been the driving force behind several of our software development projects within the last few years. This company demonstrates high professionalism in their work approach. They have continuously proved to be ready to go the extra mile. We are very happy with Belitsoft, and in a position to strongly recommend them for software development and support as a most reliable and fully transparent partner focused on long term business relationships.
Global Head of Commercial Development L&D at Technicolor