If you have ever heard about how an optimized Length of Stay (LOS) may impact the financial health of healthcare systems in theory, not in practice, you may not believe it at first glance. Reports suggest that thousands of inpatient days are saved, several thousand admissions become possible due to "sudden" bed availability (equivalent to adding dozens of new beds), and, of course, tens of millions in direct operating expenses are prevented. All of this is complemented by such "side effects" as avoiding adverse patient events (ranging from falls to multi-drug resistance and hospital-acquired infections) and reducing the total cost of care. How is this even possible? What steps do we need to follow to recreate this success?
Optimizing inpatient care, or, in particular, optimizing LOS, often means targeted interventions to improve inpatient financial performance and mitigate the financial impact of LOS challenges.
However, this is only possible if length-of-stay management relies on a specialized technical infrastructure (enterprise data warehouse) and an associated analytics platform.
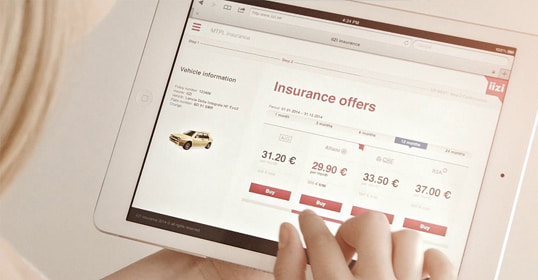
In organizations where it's implemented, clinicians have near real-time access to LOS performance metrics, updated by the minute rather than just by the day.
Challenges in Reducing Length of Stay
LOS Data is Needed Right Now, While Patients are Hospitalized
Reducing LOS by adjusting clinical decision-making is possible when providers, care team members, and leaders within a healthcare network have access to LOS data and recognize its clinical relevance. However, if manual processes are used for gathering and sharing LOS data (which are typically very resource-intensive), it can take several weeks or even months before this data is disseminated across the organization. By then, patients may have been discharged long ago, making the data useless for clinicians.
Calculating LOS in Whole Days is Inaccurate
If calculating and reporting LOS is based on data from financial systems and insurance claims, where it is recorded in days rather than hours, it creates confusion in the true utilization of hospital resources. The issue lies in the methodology: a patient discharged in the morning, who frees up a bed, may be recorded as having occupied the bed for a full day.
Adjusting Acuity Can No Longer Rely on Legacy Approaches
It only takes a few complex surgical patients to skew LOS numbers. The traditional method to adjust LOS for patient acuity uses CMI (Case Mix Index), based on the assigned DRG (categorize patients with similar clinical diagnoses), which is not consider all required factors that affect patient acuity and cost. As a result, LOS of a very sick patient may be compared to the LOS of a healthier patient. A doctor may be forced to discharge patients before completing their treatment in order to meet average benchmarks calculated this way.
Patients within the same diagnosis group often require similar resources and share comparable clinical complexity. Grouping patients by similar diagnoses (MS-DRGs) and comparing their LOS to the GMLOS (a national average for each diagnosis group) provides a more accurate way to determine whether a patient’s LOS is appropriate. Dividing each patient’s actual LOS by the MS-DRG-specific GMLOS better highlights areas where LOS is either above or below the expected standard, helping to identify opportunities for reduction.
Missing Discharge Information Increases LOS
The common practice is that social workers and nurses don’t know when particular patients are ready to leave the hospital or what the anticipated discharge date is, leaving them with little time to prepare for the patient’s discharge. This often leads to spending more time ordering medical equipment, finding a bed in a nursing facility, or confirming a ride, delaying the patient’s discharge (unnecessary hospital stays).
What Benefits to Expect After Implementing Length of Stay Analytics
Performance reports reveal insights that completely shift the focus of LOS improvement initiatives.
For example:
- It’s possible to estimate cost savings per day through automated calculations based on complex formulas.
- The ability for providers to view their own performance levels (e.g., LOS differences due to practice pattern variation) motivates them to achieve higher performance.
- When clinically relevant near real-time data is available, hospitalists become more engaged, leading to reduced practice pattern variation through clinical transformation (ultimately reducing LOS systematically).
- Finally, it’s possible to create a discharge planning process where the team is consistently informed about both the anticipated discharge date and the actual timing of discharge orders.
Or more specific findings, such as:
- Hospitalists often complete discharge orders in the early morning, but patients are discharged only later in the day. This highlights an opportunity to reduce LOS.
- LOS may vary by the day of the week, especially on weekends, due to limited availability of diagnostic procedures and challenges in discharging patients to specialized nursing facilities.
How Belitsoft Can Help
Belitsoft is an outsourcing company that specializes in healthcare software development. We help top healthcare data analytics companies build robust data operating systems.
For integrated data platforms developed to collect, store, process, and analyze large volumes of data from various sources (Electronic Medical Records, clinic management systems, laboratory systems, financial systems, etc.), we:
- Automate processes for data cleansing, standardization, and normalization.
- Configure scalable data warehouses.
- Set up and implement analytical tools for creating dashboards, reports, and data visualizations.
- Ensure a high level of data security and compliance with healthcare regulations such as HIPAA.
- Integrate machine learning and AI into analytics.
We also help build:
- Inpatient data marts (to hold patient information from EHR, including data on demographics, diagnoses, timestamps throughout care processes and pathways, and billing information)
- Inpatient dashboards, which do not require significant technical skills to segment the population (by “method of arrival,” “discharge destination,” “clinical service line,” “discharge unit,” “ICU utilization,” and other variables), but provide the possibility to create detailed reports in near real-time and export them for distribution.
If you're looking for expertise in data integration, data infrastructure, data platforms, HL7 interfaces, workflow engineering, AWS development, or data analytics, we are ready to serve your needs. Contact us today to discuss your project needs.
Rate this article
Recommended posts
Portfolio


Our Clients' Feedback








































Belitsoft has been the driving force behind several of our software development projects within the last few years. This company demonstrates high professionalism in their work approach. They have continuously proved to be ready to go the extra mile. We are very happy with Belitsoft, and in a position to strongly recommend them for software development and support as a most reliable and fully transparent partner focused on long term business relationships.
Global Head of Commercial Development L&D at Technicolor